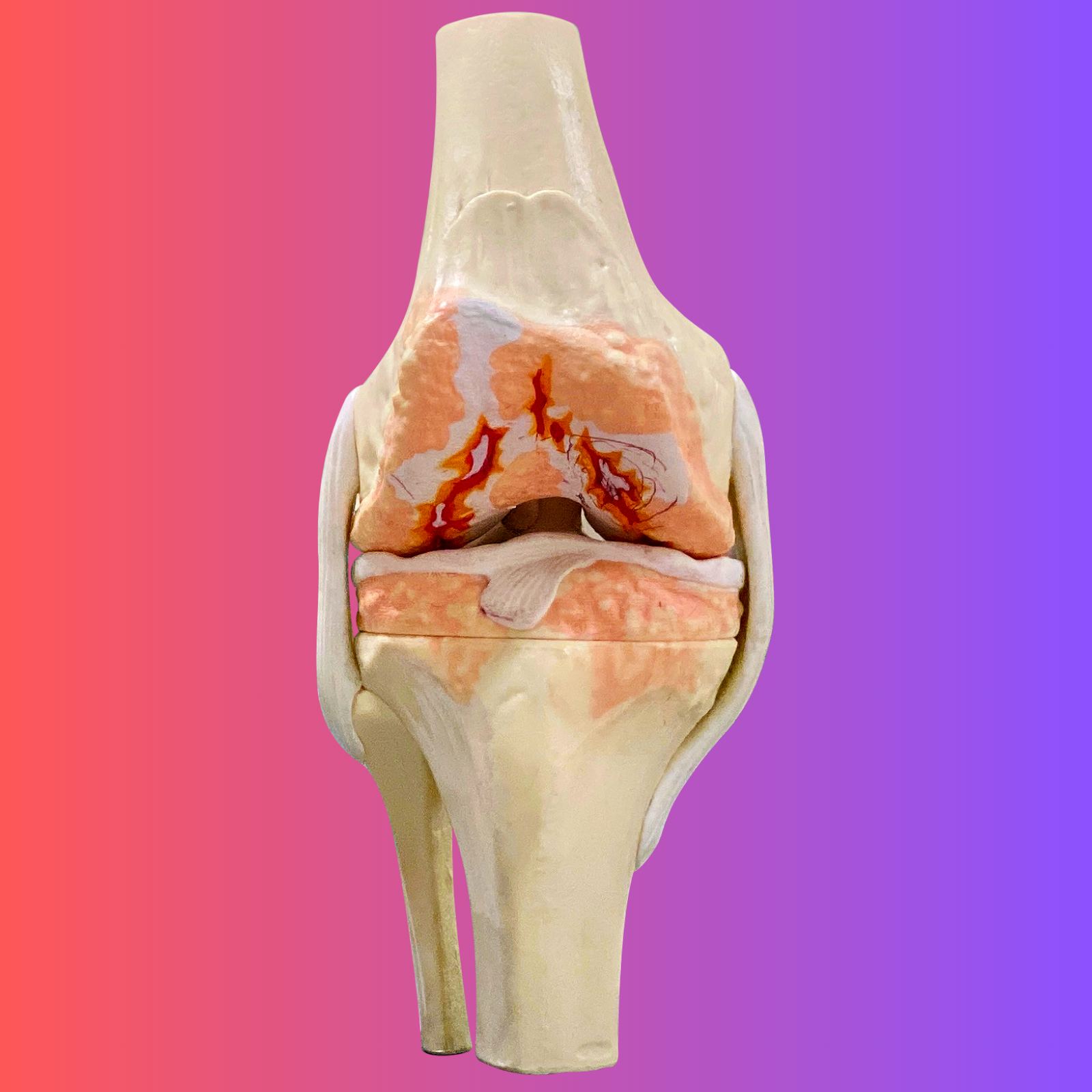
Knee joint is one of the most important joints in our body. It is also the body part taking the most load during our daily activities. There are common conditions causing severe damage of knee joint:
Risks of the below complications are uncommon, the total risk might be below 5%. Your doctor will take all the necessary steps to minimise these risks:
The purpose of total knee replacement surgery is to relieve pain, correct deformity, improve range of movement of your damaged knee joint and therefore improve your quality. Here reason why you need Total Knee Replacement:
Knee joint is one of the most important joints in our body. It is also the body part taking the most load during our daily activities. There are common conditions causing severe damage of knee joint:
Risks of the below complications are uncommon, the total risk might be below 5%. Your doctor will take all the necessary steps to minimise these risks:
The purpose of total knee replacement surgery is to relieve pain, correct deformity, improve range of movement of your damaged knee joint and therefore improve your quality. Here reason why you need Total Knee Replacement:
If your knees are constantly painful, swollen, warm, stiff, tender, or visibly deformed—and your movement feels limited or unstable—these signs usually indicate advanced joint damage that meets the criteria for surgery.
If lifestyle changes, painkillers, anti-inflammatory medicines, joint-protective medicines, or hyaluronic acid injections haven’t given meaningful relief, it’s a strong signal that non-surgical options are no longer effective.
Yes. Your surgeon will assess your knee, explain the current condition, and walk you through why TKR is recommended and what outcomes you can expect.
Absolutely. You should know what the procedure involves, what happens during hospitalisation, and what recovery and rehabilitation look like.
A physician will review your overall health and optimise any underlying conditions to lower surgical risks and ensure a safer recovery.
Yes. Inform them about all blood thinners, prescribed or over-the-counter, as well as any traditional or herbal remedies. These can affect bleeding and must be managed before surgery.
Any active infection—skin issues, open wounds, urinary tract infections, or respiratory infections—must be treated first. Operating with an untreated infection increases the risk of complications.
Yes. If both knees are equally damaged, doing both in a single session is common and often recommended for efficiency and recovery balance.
| Days | Activities |
|---|---|
| Day 1 | You’ll be admitted a day before surgery and seen by your orthopaedic surgeon, physician, and anaesthetist to decide on general or regional anaesthesia. Older patients may need a bone density check. You’ll sign consents for surgery, anaesthesia, and blood transfusion. Nurses will clean and prep your knee to reduce infection risk. |
| Day 2 | After your knee surgery—one or both—you’ll be monitored in the ICU for blood pressure, pulse, blood loss, and fluid balance. This close observation is especially important for older patients to ensure safety and stability. |
| Day 3 | You’ll be able to eat and drink comfortably while the rehab team helps you start bed exercises, lower limb movements, and even sitting, standing, or walking a few steps. |
| Day 4 | You’ll start standing and walking with a frame, guided by the rehab team. They’ll prepare you for home activities, helping you regain confidence in daily movements. |
| Day 5 | You’ll typically stay in the ward for 5 to 7 days. If you’re confident managing at home, regular physiotherapy may not be needed; otherwise, your doctor will arrange follow-up care. |

Upon discharge, you will be given oral antibiotics, painkillers, and anti-inflammatory medicines. Additionally, keep the wound dressing dry and avoid changing it yourself.
Meanwhile, you are encouraged to do ice pack massage on the operated knee. Cold therapy helps reduce swelling, warmth, pain, and tenderness, which in turn makes it easier to exercise and mobilise your knee comfortably.
Subsequently, you will have a review appointment accordingly. Your doctor will check the wound, remove stitches, and advise if further physiotherapy is needed.
Finally, if your bone density check shows osteoporosis or low bone mass, treatment will be recommended so that your bone quality improves and consequently ensures your implants remain stable for the long term.
